Sections
- Antibiotics
- Artificial Sweeteners
- Aspirin & Stroke
- Blood Pressure Medications & Mineral Depletion
- Calcium
- Coenzyme Q10
- Diet & Lifestyle
- Food Allergies
- Nutritional Frontiers Purity & Potency
- Possible Imbalances From Medications
- Quality & Patented Research
- Quality, Purity, & Potency
- Targeted Nutrition
- The Benefits of Multivitamin Use Substantiated
- The Dangers of Over-The-Counter Pain Medications
- The Ins & Outs of Whey Protein
- Vitamin D Deficiency
- What’s In Your Multivitamin?
- Why Choose Nutritional Frontiers Vegetable Protein Over Competing Brands
Many people are concerned about vitamin D these days. Vitamin D is a fat-soluble vitamin that the body produces when the skin is exposed to ultraviolet light (specifically UVB) from the sun.
The skin, the liver, and the kidneys are all involved in vitamin D production. Vitamin D3, also called cholecalciferol, is made in the skin when a cholesterol-based compound in our body called 7-dehydrocholesterol reacts with ultraviolet light. Cholecalciferol, whether made in the skin from sun exposure or ingested as a supplement, is then turned into 25-hydroxycholecalciferol by the liver. This substance is then bound to a protein in the blood and carried to the kidneys, where it forms calcitriol (also called 1,25-dihydroxycholecalciferol).
Calcitriol binds to vitamin D receptors in the body and mediates the physiological actions of vitamin D. If your doctor orders a blood test to check your vitamin D levels, you will likely see several of these names on the blood test results. The most important one to look at clinically is 25-hydroxyvitamin D, sometimes called “25 (OH)D.”

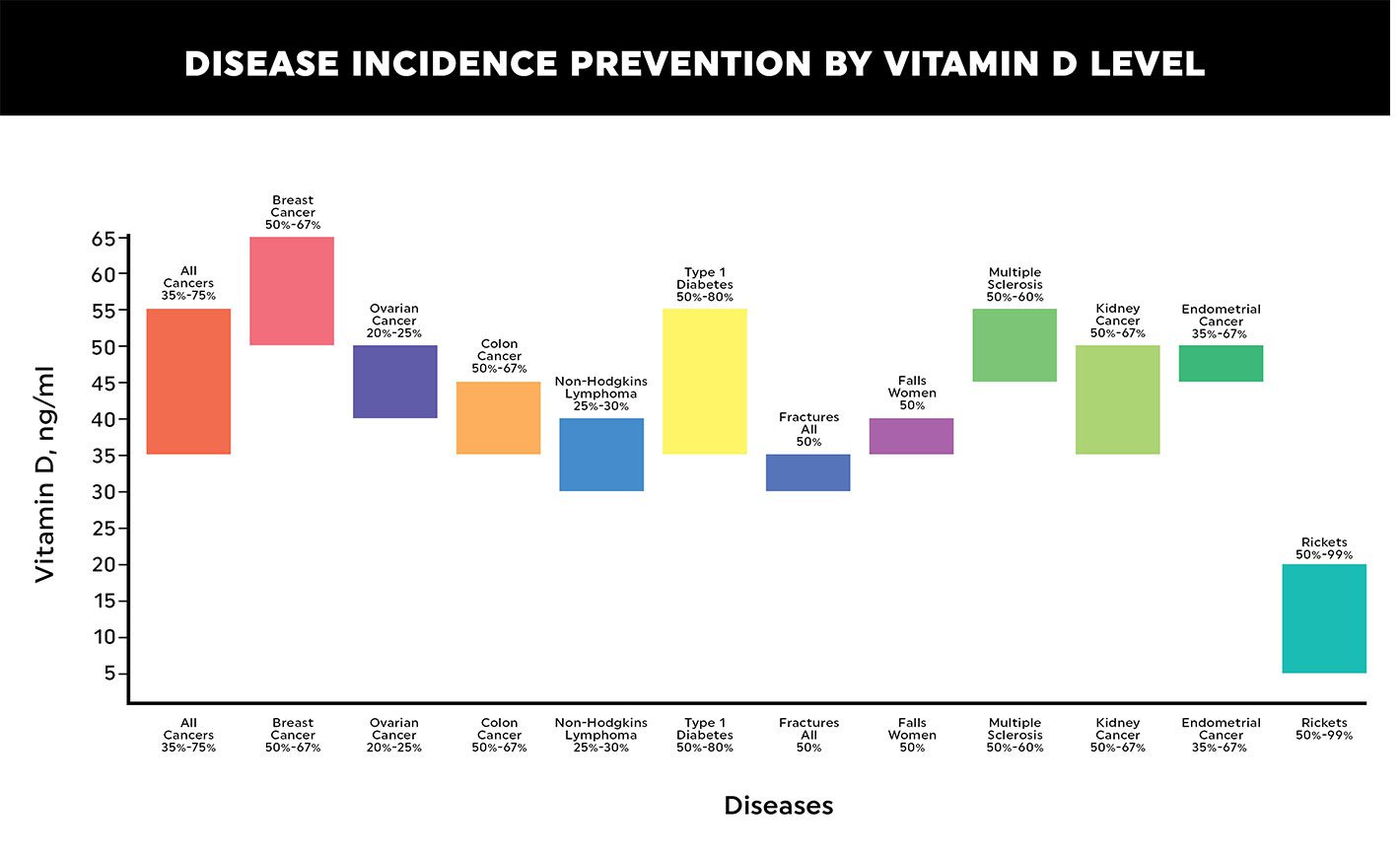
The ideal reference range for vitamin D blood tests is debated in the medical community. The Vitamin D Council proposes an optimal reference range of 25(OH)D of 50-80 ng/mL (125-200 mol/L). This is higher than the typical laboratory value of 30 ng/mL (70 nmol/L), which the Vitamin D Council considers to be outdated and not reflective of the latest research on vitamin D deficiency. If your blood test shows that you are deficient in vitamin D and you start to take a supplement, you should get your 25 (OH)D levels retested every few months to assess the adequacy of your dosing regimen.
Vitamin D deficiency can be prevalent in certain populations, geographical locations, and is also noticed in several disease states. Since sun exposure is necessary for endogenous (‘within the body’) vitamin D production, sunscreen can reduce the ability of the body to synthesize vitamin D from sun exposure. This occurs only when the sunscreen is applied liberally and frequently, though. More and more people are avoiding sun exposure due to fears of skin cancer or depletion of the ozone layer.
Also, many people work indoors during the day and in that way do not get as much sun exposure as necessary for vitamin D production. Combine these elements with living in a northern latitude where adequate sun exposure is limited to a few months of the year and you are left with many people who would likely benefit from vitamin D supplementation.
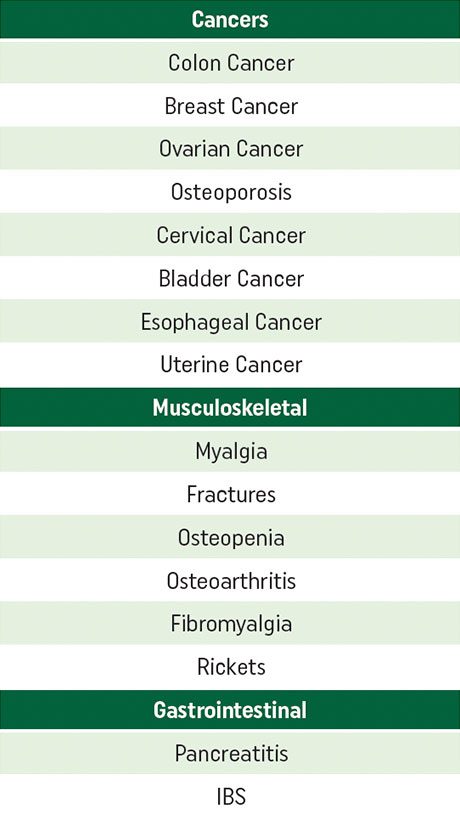
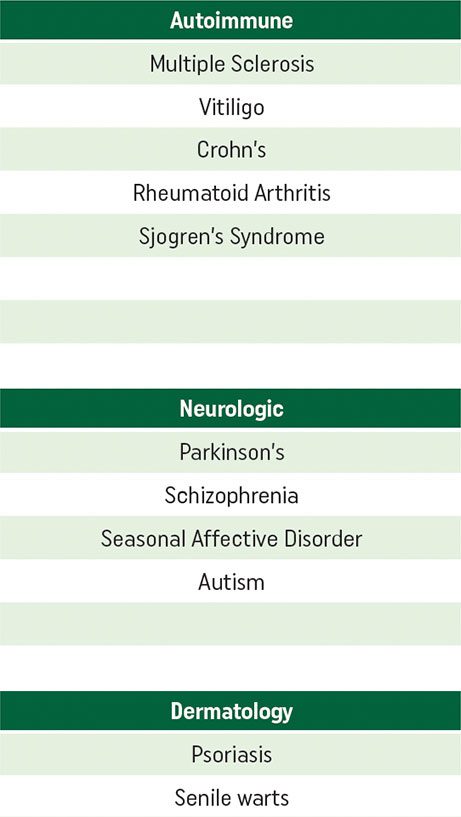
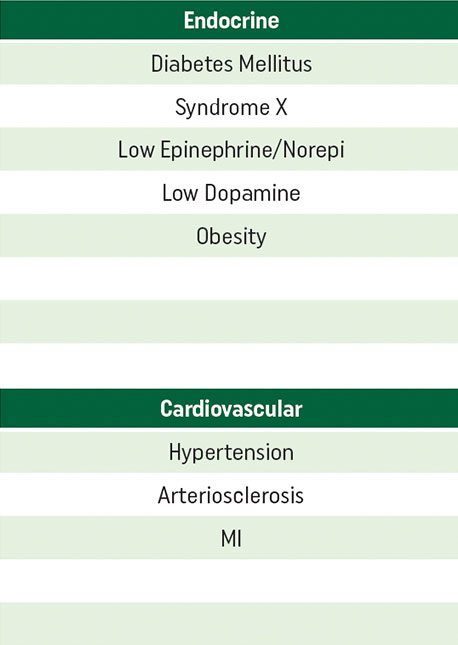
Many diseases are associated with low vitamin D status, including the following:
- Cancer of the colon, breast, ovaries, cervix, uterus, esophagus, bladder
- Osteoporosis and osteopenia
- Multiple sclerosis
- Vitiligo
- Crohn’s disease
- Rheumatoid arthritis
- Tuberculosis
- Diabetes
- Syndrome X / Metabolic Syndrome
- Psoriasis
- Pancreatitis
- SAD (Seasonal Affective Disorder)
- Parkinson’s
- Sjogren’s syndrome
- Schizophrenia
- High blood pressure
- Arteriosclerosis
- Fibromyalgia
- Osteoarthritis
- Autism
- IBS
Vitamin D is a fat-soluble vitamin that is essential for maintaining normal calcium metabolism. Vitamin D3 (cholecalciferol) can be synthesized by humans in the skin upon exposure to ultraviolet-B (UVB) radiation from sunlight, or it can be obtained from the diet.
Nutritional Frontiers Vitamin D Supplements
We offer 3 different products containing a range of vitamin D dosing and delivery methods to meet your needs.
Conditions Associated with Suboptimal Vitamin D Status
References:
All Cancers: Lappe JM, et al. Am J Clin Nutr. 2007;85:1586-91. Breast: Garland CF, Gorham ED, Mohr SB, Grant WB, Garland FC. Breast cancer risk according to serum 25-Hydroxyvitamin D: Meta-analysis of Dose-Response (abstract). American Association for Cancer Research Annual Meeting, 2008. Reference serum 25(OH) D was 5 ng/ml. Garland, CF, et al. Amer Assoc Cancer Research Annual Mtg, April 2008. Colon: Gorham ED, et al. Am J PREV Med. 2007:32:210-6. Diabetes: Hypponen E, et al. Lancet 2001:358:1500-3 Endometrium: Mohr SB, et al, Prev Med. 2007:45:323-4, Falls: Broe KE, et al. J Am Geriatr Soc. 2007:55:234-9. Fractures: Bischoff- Ferrari HA, et al. JAMA. 2005:293:2257-64. Heart Attack: Giovannucci et al, Arch Intern Med/Vol 168 (No11) June 9, 2008.
Multiple Sclerosis: Munger KL, et al. JAMA. 2006:296:2882-8. Non-Hodgkin’s Lymphoma: Purdue MP, et al. Cancer Causes Control, 2007;18:989-99 Ovary: Tworoger SS, et al. Cancer Epidemiol
Biomarkers Prev. 2007;16:763-8. Renal: Mohr SB, et al. Int J Cancer. 2006;119:2705-9. Rickets: Amaud SB. et al. Pediatrics. 1976 Feb;57(2):221-5.
**All percentages reference a common baseline of 25 ng/ml as shown on the chart.